Could halting CAG expansions be a new treatment for HD?
The gene MSH3 is getting a lot of attention in HD research lately. New findings suggest MSH3 lowering could halt CAG repeat expansions, offering a new therapeutic avenue.
By Dr Sarah Hernandez October 05, 2023 Edited by Dr Leora Fox
A recent paper from a group at UMass Chan Medical School, spearheaded by Dr. Daniel O'Reilly and led by Dr. Anastasia Khvorova, used genetic strategies to lower a protein other than huntingtin. This time the researchers went after a gene called MSH3. This is a gene that’s been getting a lot of attention in Huntington’s disease research as of late. So what’s all the hype about? And does this mean we’ve abandoned huntingtin lowering?
CAG stutter
One of the most interesting findings in HD research in the past several years has been something called “somatic instability,” which is also sometimes called “somatic expansion.” It refers to the perpetual expansion of the CAG repeat in “somatic” cells, or cells of the body. You can think of it like a molecular stutter of the CAGs in the huntingtin gene.
This ongoing expansion doesn’t happen in all cells though. The CAG repeats appear to be quite stable in certain cells and tissues, like blood. So that means if someone has a genetic test on their blood at the age of 18, the number of CAG repeats will very likely be the same when they’re 50, and remain unchanged throughout life. However, certain cells appear to gain CAG repeats throughout one’s life. Those cells tend to be the exact ones that are most vulnerable in HD – brain cells.
In 2003, Dr. Peggy Shelbourne carried out ground-breaking work using brain samples generously donated by people who had died from HD. Her work showed that specific areas of the brain have massive CAG expansions – up to 1000 CAG repeats! Those people certainly weren’t born with CAG repeats that big, which means that they were acquired over their lifetimes.
Interestingly, the brain region that had those massive CAG repeat expansions was also the most vulnerable to HD – an area called the striatum. For many years after this discovery, it wasn’t clear how these CAG expansions were happening or what it meant for HD progression.
What controls age of onset?
Then, in 2015, another ground-breaking paper was published, this time by the Genetic Modifiers of Huntington’s Disease (GeM-HD) Consortium. This was a huge study that looked at the entire genetic makeup of over 4,000 people with HD. This gave the researchers lots and lots of data, the richest sample of genetic information that the world had ever had from individuals with the gene for HD.
“Certain cells appear to gain CAG repeats throughout one’s life. Those cells tend to be the exact ones that are most vulnerable in HD – brain cells. ”
The GeM-HD Consortium was interested in trying to find small genetic changes that may contribute to how early or late someone started to get symptoms of HD – genes we call “genetic modifiers.” Identifying variants that modify the age of symptom onset could uncover targets for therapeutics.
What the Gem-HD Consortium found knocked everyone’s socks off. The modifier genes that changed the age of symptom onset were almost all involved in a single biological process! Finding modifiers that clustered together like this was completely unexpected, but was also incredibly telling. The genes were involved in a process called DNA repair.
Molecular proofreaders
Proteins are the molecular machines that run our cells, and they are made using genetic messengers, RNA, which in turn are created from our DNA. Every time a new protein needs to be produced or refreshed, there’s an opportunity for mistakes in the process. DNA repair molecules are the proofreaders that check for mistakes. To ensure that there are no mistakes in that translation process from DNA to protein, these molecular proofreaders (aka DNA repair molecules) check that message.
Sometimes there are small genetic changes in DNA repair genes that cause them to function better or worse. Really great DNA repair genes do an excellent job proofreading the huntingtin gene, so no mistakes are made when the protein is made, and CAG repeat sizes remain stable. But DNA repair genes that are prone to making mistakes while proofreading may lose track of how many CAGs should be translated. This can mean that errors slip through, increasing the CAG repeat length over time.
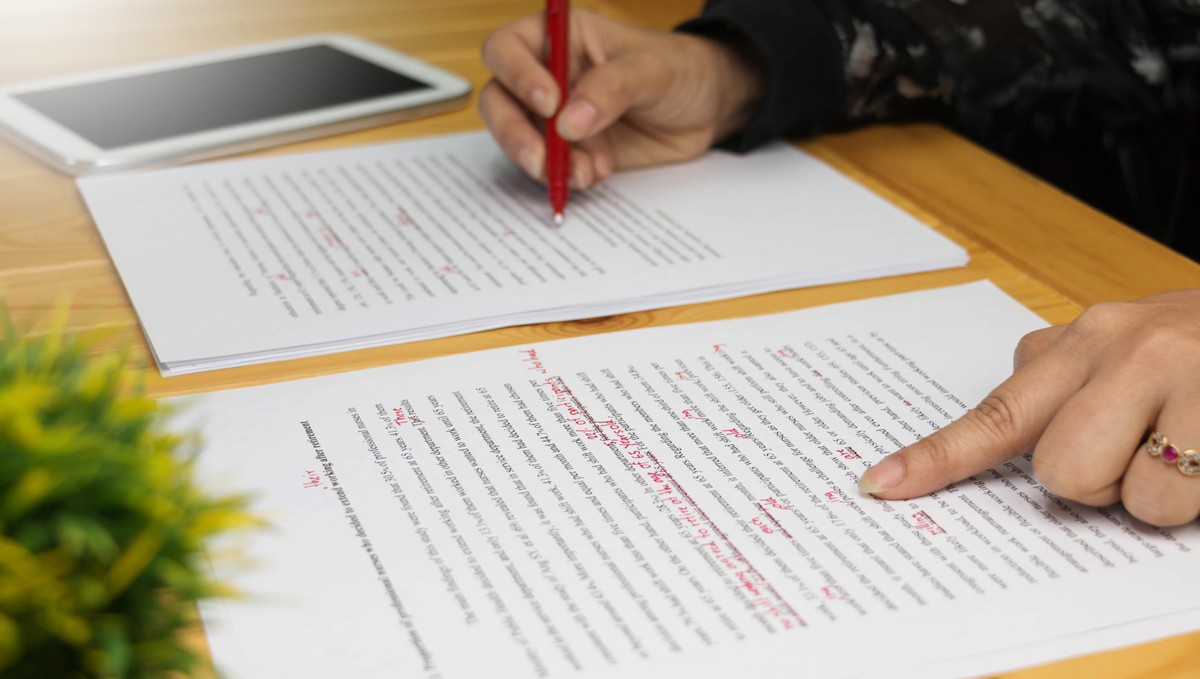
The GeM-HD Consortium study showed that some people had tiny genetic differences that likely made their DNA repair genes better proofreaders, leading to later symptom onset. This finding finally added some perspective to Dr. Peggy Shelbourne’s work, linking DNA repair genes to the somatic expansion observed in the brains of people who had died from HD. Researchers remain very excited by this because it suggests that if we can control expansion of the CAG repeat, we may be able to delay HD symptom onset.
Targeting MSH3 controls CAG stutters
Scientists are now targeting DNA repair genes in various animals that model HD. One gene of interest is called MSH3. HDBuzz recently wrote about MSH3, its molecular partners, and their involvement in CAG expansion, which you can read about here. MSH3 proofreads the type of genetic structure that is created by CAG repeats. Scientists have been successful in blocking CAG repeat expansion by lowering levels of MSH3. They’ve used genetic methods similar to those used for lowering huntingtin.
Work led by Dr. Khvorova in a recent publication has now taken the next step, seeing if silencing MSH3 with a drug in mice that model HD has the same effect as genetic manipulation. Their drug delivers a small piece of genetic material that targets and silences MSH3 in the brain. Excitingly, they find that a single dose of their MSH3-targeting drug delivered to the brain can block CAG repeat expansion for up to 4 months in various models of HD mice!
While the potential for a drug that blocks somatic expansion is exciting, the authors acknowledge the need for more safety studies before their drugs targeting MSH3 can move into people. This new study shows that their drug only targets the MSH3 messenger molecule, sparing other genes. However, additional studies are needed to determine if other DNA repair genes are affected at the protein level. They also note the importance of long term safety studies to ensure their drugs aren’t having damaging effects on brain cells. Follow up experiments will also be needed to determine if reducing somatic instability improves HD-like symptoms in mice.
“They find that a single dose of their MSH3-targeting drug delivered to the brain can block CAG repeat expansion for up to 4 months in various models of HD mice! ”
Expanding our targets
While other targets, like MSH3, are welcome in our conquest against HD, it doesn’t mean that huntingtin is being abandoned as a target. We, without doubt, know the single cause of HD lies with the huntingtin gene. So it still makes sense to design drugs that go after the root cause of the disease. In that vein, trials by Roche, Wave Life Sciences, and Vico Therapeutics testing their huntingtin-lowering drugs march on.
If experiments in mice that target MSH3 are successful though, having combinatorial therapies that go after the root cause while also blocking CAG repeat expansion could be the one-two punch needed for HD. We’ll no doubt be hearing lots more about DNA repair genes (molecular proofreaders) in HD research, and will likely see trials in the near future that target CAG expansions.