Bone marrow transplantation in Huntington's Disease
Bone marrow transplant protects HD mice from some symptoms, suggesting the immune system may be an important target
By Dr Tony Hannan January 04, 2012 Edited by Dr Jeff Carroll
Are there connections between the body’s immune system and the progression of Huntington’s disease? New evidence suggests that correcting changes in the immune system could have real impact on brain aspects of HD.
Huntington’s disease as a brain disease
When the brains of people who’d died of Huntington’s disease were first studied, the most striking observation was that many cells in a part of the brain called the striatum had died during the degenerative process. In fact, there were almost holes in the brain where the striatum should have been.

Like many areas of science and medical research, early findings greatly influence researchers who come later, encouraging them to first ‘look under the lamp-post’ rather than into the darker nooks and crannies which have yet to be explored. Much HD research has focused on what’s wrong in the striatum, but is that the whole story?
As we look more and more widely it has become increasingly clear that HD is not just a disease of the striatum, or even the basal ganglia, but can affect other parts of the brain such as the cerebral cortex (which may be particularly important for the thinking and emotional symptoms).
However, in recent years it also become apparent that HD pathology is not only restricted to the brain - it can also occur in other organs and systems of the body.
The immune system in HD
Each and every cell in our body contains the HD gene, and in people with an expanded HD gene, the abnormal huntingtin protein is found in every cell, too.
The latest revelation in this journey of discovery has just been published by Wanda Kwan, Paul Muchowski and colleagues in the Journal of Neuroscience.
Muchowski and colleagues were following up on recent evidence that the immune system is dysfunctional in HD. The immune system is crucial in protecting the human body from germs.
In the past, scientists have considered the brain ‘immune privileged’, meaning that the brain was separated from the rest of the body’s immune system. But recent discoveries suggest that the central nervous system (with the brain as its crowning glory) and the immune system share a complex relationship. In fact, brain-immune communication goes both ways - the body’s immune system can change the brain, and changes in the brain can be reflected in the immune system.
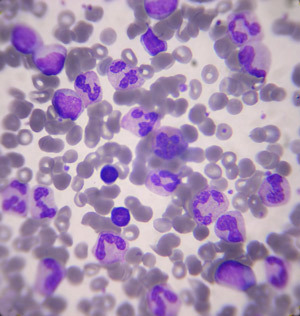
A previous study, involving Maria Bjorkqvist and Sarah Tabrizi who are also co-authors on this new paper, of blood samples from HD mutation carriers and symptomatic HD family members, focused on the molecules that regulate the state of the immune system. This study revealed that specific molecules show early changes in HD subjects compared to control volunteers without the HD mutation.
Like virtually all changes that have been found in HD patients, these immune system molecules were also found to be altered in the blood of HD mice. Therefore the role of the immune system in HD can be tested experimentally using HD mouse models.
HDBuzz readers may recall another study by Muchowski’s group which showed that a drug known as JM6 altered symptoms in HD mice, despite not being transported into the brain at all. JM6 Likely works, in part, through the immune system.
Bone Marrow Transplant
Now that it’s clear that moderating the immune system can have effects on the brains of HD mice, Muchowski and colleagues have performed a clever experiment. They carried out bone marrow transplantation in HD mice, replacing the bone marrow of HD mice with bone marrow collected from healthy (‘wildtype’) mice.
The bone marrow is crucial in generating new cells for the immune system and therefore this kind of transplant would test the role of the immune system in HD. Bone marrow transplants are regularly conducted in humans whose bone marrow has been damaged, for example after chemotherapy.
Did it work?
The findings were very interesting. The HD mice which had received a transplant from healthy control mice showed some subtle, but significant, improvement in the movement problems that HD mice normally display.
Evidence that the transplantation of healthy bone marrow into the HD mice had directly affected the brains of the animals was provided by analysis of ‘synapses’, the trillions of connections that are known to occur between the billions of ‘neurons’ in the brain. When brain cells are sick or dying, they begin to lose synapses, causing major communication problems in the brain.
Bone marrow transplantation increased the number of synapses in the brain, suggesting that this change to the immune system was directly impacting the brain. This is extremely exciting, because it proves that we can provide treatments to the body that have direct impact inside the brain.
Finally, some of the aforementioned immune system molecules which are altered in HD patients and mouse models, were restored to normal levels following bone marrow transplantation. This suggests that the immune system has been, to some extent, reset to normal levels.
As the authors discuss, the effects of the healthy bone marrow transplant did not lead to full rescue of the symptoms, but rather showed ‘disease modifying’ effects. This is not surprising, as the brains of the HD mice continued to express the gene mutation and were thus exposed to the toxic effects of the huntingtin protein.
Nevertheless, this important new paper provides additional evidence that the immune system is affected in HD and that correcting immune dysfunction could have beneficial effects for patients.
It suggests new avenues for further research into the disease processes in HD and also points towards a potential clinical trial approach. It may be that we will need to target both the brain and the body, including the immune system, if we are to develop successful approaches to prevent and treat HD.